A new MRI technique can locate foci of aggressive tumour cells and could improve the treatment of glioblastoma
Brain Neoplasms,
Glioblastoma,
Magnetic Resonance Imaging,
Magnetic Resonance Spectroscopy,
Neoplastic Stem Cells,
Prospective Studies.
Anthony Lemarié teame RADOPT :Radiotherapy Optimising: from molecular signalling pathways to clinical trials
Glioblastomas are highly aggressive brain tumours whose treatment consists of surgery and radiochemotherapy. A new medical imaging technique could improve patients’ prognosis, according to a recent clinical trial led by Elisabeth Moyal, professor at Toulouse III – Paul Sabatier University and head of the radiotherapy department at the IUCT-Oncopole. The results of her clinical trial, conducted at Oncopole and within her Inserm research team at the Toulouse Cancer Research Centre (CRCT – Inserm/CNRS/UT3), in collaboration with the neurosurgery department of Toulouse University Hospital, were published in the journal Science Advances on November 3.
The treatment for glioblastoma consists of surgical resection of the central tumour zone (known as the EC zone), followed by radiochemotherapy in the same region, as well as in the large peritumoral zone infiltrated by the tumour cells that have migrated there (known as the FLAIR zone). Despite this treatment, most patients will suffer a relapse, particularly in these FLAIR peritumoral areas that were not removed during the initial surgery.
It is these high-risk areas that have been studied by Prof Elisabeth Moyal and her Inserm team. Using an MRI technique known as magnetic resonance spectroscopy, which analyses the metabolism of tumours, the team had previously shown that EC and FLAIR peritumoral tumour regions displaying hypermetabolism predicted where the tumour would recur after treatment.
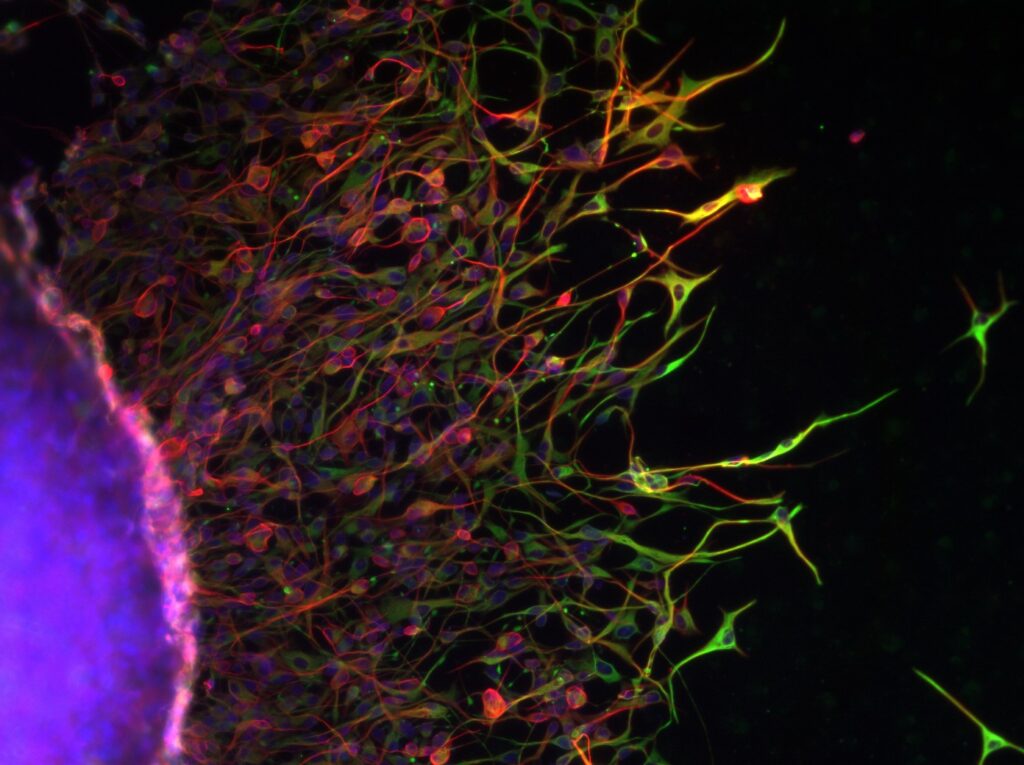
Recurrence is mainly attributed to a subpopulation of more aggressive tumour cells, the glioblastoma stem cells. The researchers’ hypothesis was therefore that the hypermetabolic regions were enriched in this population of cancer stem cells.
To test this hypothesis, a clinical trial was set up in 16 patients with glioblastoma, who underwent preoperative conventional MRI combined with magnetic resonance spectroscopy, enabling biopsies to be taken from CE and FLAIR tumour areas, whether hypermetabolic or not, during surgery guided by these MRI techniques. Patients were then treated with standard radiochemotherapy.
The experiments carried out at the CRCT by Dr Anthony Lemarié, senior lecturer at UT3, and Caroline Delmas, laboratory engineer at the IUCT and the CRCT, confirmed their hypothesis and demonstrated that the hypermetabolic zones in the FLAIR peritumoral regions were enriched in glioblastoma stem cells and overexpressed many genes involved in tumour aggressiveness and resistance. The greater the enrichment of glioblastoma stem cells in these hypermetabolic peritumoral areas, the more severe the prognosis for relapse.
“The combination of two imaging techniques, MRI and magnetic resonance spectroscopy, prior to surgery, could enable better resection and therapeutic targeting of the hypermetabolic areas present in the peritumoral regions,” explains Prof Elisabeth Moyal. This specific targeting could improve the prognosis of these very aggressive brain tumours.
Glioblastoma stem cells migrating from a tumour structure. Credit: Caroline Delmas
Discover the published article
Science Advances, 3 novembre 2023 – Vol 9, Issue 44
The STEMRI trial: Magnetic resonance spectroscopy imaging can define tumor areas enriched in glioblastoma stem-like cells
Anthony Lemarié, Vincent Lubrano, Caroline Delmas, Amélie Lusque, Juan-Pablo Cerapio, Marion Perrier, Aurore Siegfried, Florent Arnauduc, Yvan Nicaise, Perrine Dahan, Thomas Filleron, Muriel Mounier, Christine Toulas, Elizabeth Cohen-Jonathan Moyal